Frugally designed system, evaluated in mice, aims to improve access to fluorescence-guided surgery
Cutting-edge surgical tools are often made with state-of-the-art technology, which can limit their overall accessibility. In an effort to expand surgical options for tumor removal, an NIBIB-funded team is developing a compact fluorescence-guided surgery system crafted from cost-effective, off-the-shelf components, an advance that could significantly reduce costs compared with current commercially available approaches. Their frugally designed system was evaluated in a mouse model and was recently reported in the Nature journal Scientific Reports.
“How can we level the playing field across different hospital systems?” asked senior study author Samuel Achilefu, Ph.D., professor and chair in the Department of Biomedical Engineering at the University of Texas Southwestern Medical Center. “Many clinical centers don’t have access to advanced surgical tools, which can potentially shape patient outcomes. With a cost-effective approach, our team aims to make an accessible real-time fluorescence system that highlights tumors in a similar fashion across all hospitals, no matter their location or budget.”
Focusing on fluorescence-guided surgery
How does fluorescence-guided surgery work? In the context of cancer, the first step is to administer a contrast agent that specifically targets tumors. This agent, called a fluorophore, is activated when it’s exposed to certain types of light, causing it to glow. In this way, a surgeon can see how far the tumor extends, allowing them to fully remove the cancer while sparing healthy tissue. They can also see if any malignant material is left behind during the course of the surgery.
Many different fluorophores are being explored, and some are activated when they are exposed to visible light, making them detectable to the naked eye. But like the glow of a firefly, this fluorescence is most easily seen when it’s dark, and turning off the lights in the operating room is not an ideal solution.
To overcome this obstacle, researchers are investigating fluorophores that are activated when they are exposed to near-infrared light. Near-infrared light lies just beyond the visible spectrum and can travel farther through tissues, meaning that surgeons can better detect tumors deep in the body. The catch, of course, is that humans can’t see near-infrared light—not without the proper tools, anyway.
“When a near-infrared fluorophore glows, you can’t see it with your eyes,” explained lead study author Leonid Shmuylovich, M.D., Ph.D., assistant professor of medicine and radiology at Washington University in St. Louis. “You need a special camera that’s sensitive to those wavelengths, and then you need a way to project that signal so that the surgeon can see it,” he said. In existing systems, this signal is typically displayed to the surgeon on a nearby screen.
While several different near-infrared fluorescence-guided surgical systems have been approved for a variety of indications, they have two major limitations that hinder their widespread use: size and cost. “Existing systems have a large footprint in the OR, and some require assistance by another user to navigate the device, which may hinder a surgeon’s normal workflow,” noted Achilefu. “Not to mention the large price tag associated with these systems, which can cost $100,000 or more,” he added.
Cutting costs, streamlining size, optimizing design
For many years, research in the Achilefu lab has included the ongoing development of a low-cost, fluorescence-guided surgical system that uses goggles to visualize the fluorescent signal. Instead of viewing the tumor’s fluorescence on a nearby screen, this augmented reality approach projects the near-infrared signal directly onto an eyepiece, superimposing the illuminated tumor over the surgeon’s field of view.
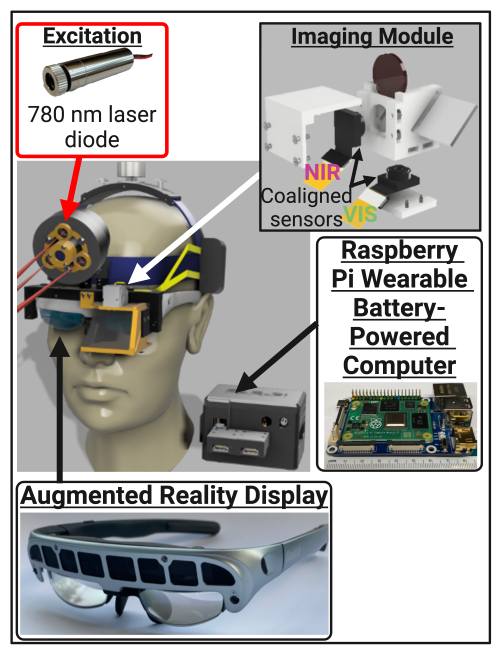
Building on previous research, the team has introduced their latest model, built from entirely off-the-shelf components and simple 3D-printed pieces. Their system has the following major components: sources of visible and near-infrared light (similar to simple laser pointers), a minimal camera system and processor, and commercial augmented reality glasses. These disparate parts are joined together using 3D-printed mounts, with the entire unit sitting on top of the user’s head. Along with the processor, a battery pack to power the unit sits on the user’s waist, making the system untethered and completely hands-free. The individual components of the system cost approximately $1,000, and the researchers hope that a commercial model would be a fraction of the cost of currently available systems.
“We wanted to see if the most basic camera system was capable of detecting a near-infrared signal, and to our surprise, it actually outperformed our previous designs,” said Shmuylovich, who completed this research during a postdoctoral fellowship in the Achilefu lab at Washington University in St. Louis. “With some tinkering, we were able to customize the system to filter out background signals, providing the core functionality for a fluorescent-guided system.”
The placement of the cameras represented an important advance, Shmuylovich explained. Many technologies that superimpose an image over another—in this case, the fluorescent signal on top of the surgeon’s field of view—suffer from something called the parallax effect. This is where the overlaid image is not perfectly aligned with reality. To help overcome this effect, the researchers employed a beamsplitter (a device that separates incoming light into two separate paths). They placed the beamsplitter in front of the augmented reality glasses and placed the camera just above the user’s eye in line with the light bouncing off the beamsplitter. “This way, the light goes either through the beamsplitter into the user’s eye, or it bounces off the beamsplitter into the camera,” Shmuylovich explained. “This dramatically improves the optical alignment of our system and was a really exciting innovation,” he said.
Evaluating performance
The team benchmarked their device with more than 10 existing fluorescence-guided systems, reviewing published values of features like fluorescence sensitivity, resolution, and irradiance (brightness). Despite the diminished size and cost of their system, the researchers found that their frugally designed goggles had comparable specifications to products on the market. They also evaluated the real-world utility of their system and performed surgery in mice bearing breast tumors. “With our system, we can see the tumors, remove them, and if there is any residual tumor left, we can see it in real time,” said Achilefu.
The researchers stressed that this technology is a template and not a finished product. “This is a tool; this is the beginning,” said Shmuylovich. “We wanted to show that low-cost components, when creatively combined, can rival the performance of expensive and established technologies,” he said.
Qi Duan, Ph.D., program director in the Division of Health Informatics Technologies at NIBIB, agreed: “Through their innovative engineering approach, this team has laid the foundation for an accessible fluorescence-guided surgical system,” he said. “With its open-source and inexpensive design, this resourceful technology could be adapted for multiple fluorescence-guided applications and could someday help improve surgical care.”
This study was supported in part by grants from NIBIB (R01EB030987 and T32EB021955), the National Cancer Institute (P30CA091842), and the NIH Office of the Director (S10OD027042).
This science highlight describes a basic research finding. Basic research increases our understanding of human behavior and biology, which is foundational to advancing new and better ways to prevent, diagnose, and treat disease. Science is an unpredictable and incremental process—each research advance builds on past discoveries, often in unexpected ways. Most clinical advances would not be possible without the knowledge of fundamental basic research.
Study reference: Shmuylovich, L., O’Brien, C.M., Nwosu, K. et al. Frugal engineering-inspired wearable augmented reality goggle system enables fluorescence-guided cancer surgery. Sci Rep 14, 24402 (2024). https://doi.org/10.1038/s41598-024-75646-0
