Multi-level implants designed to regenerate complex tissues
Repairing injured tissues, like knee cartilage, with cell-seeded implants is a promising approach for tissue regeneration. Now, NIBIB-funded bioengineers in the Rice Biomaterials Lab have created a 3D-printed scaffold designed to support the growth of complex tissues composed of different layers of cell types with different structural properties and functions.
The team was led by Antonios G. Mikos, Ph.D., the Louis Calder Professor of Bioengineering, Chemical and Biomolecular Engineering at Rice University, Houston, TX. The work is reported in the scientific journal, Bioprinting.1

The Rice team and others in the field have previously developed 3D-printed scaffolds that carried a slurry of a single cell type. However, injured regions, such as bone and cartilage are actually made up of different types of cells and tissues, often arranged one layer on top of the other with each layer having different biological and mechanical properties.
“This new technology allows us to print multi-layered scaffolds seeded with different cell types in each layer,” explained Mikos. “The aim is to grow tissues that better mimic the original structure to create a more functional and durable repair.”
The 3D-printing system is unique in several respects. The implant is made of a thermoplastic that is printed in layers of threads that resemble miniature Triscuit crackers, with their “threads” arranged in alternating layers. These thermoplastic threads provide strong mechanical strength. The system also etches thin canals within each thread. The canals are designed to carry the different cell types needed to promote the growth of repair tissues when implanted.
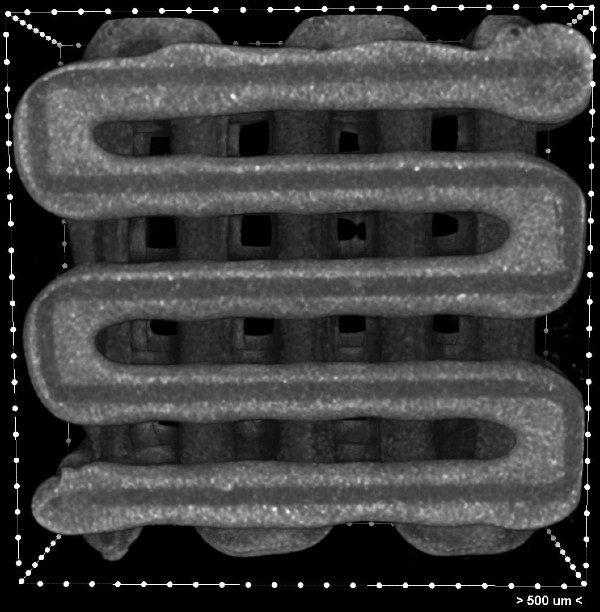
The scaffold is built with rapidly cooling thermoplastic so after etching the tiny canals, a bioink containing the desired cell types can be safely and gently deposited into each layer of the implant. Quick cooling also allows for the addition of temperature-sensitive bioactive molecules that promote the growth of the implanted cells.
“The major innovation here is our ability to spatially load a scaffold that is 3D printed with different cell populations and with different bioactive molecules,” says Mikos.
The prototype implant is currently being rigorously tested to maximize biocompatibility and to optimize the viability of cells and bioactive compounds in the device over time. The group is also working on using imaging to measure the exact size and shape of the target damaged area -- for example, in the knee cartilage of a patient. Those data will be used to program the 3D-printer to create layered implants that fit precisely into the damaged site.
This work was supported by the National Institute of Biomedical Imaging and Bioengineering (P41 EB023833), Consellería de Cultura, Educación e Ordenación Universitaria, the Robert and Janice McNair Foundation MD/PhD Student Scholar Program, and a Rubicon postdoctoral fellowship from the Netherlands Organization for Scientific Research.
