In recognition of International Women’s Day (March 8), we’re featuring a bioengineer who has inspired inclusion (this year’s theme) by her global contributions to women’s health.
Rebecca Richards-Kortum, Ph.D., a professor of bioengineering at Rice University in Houston, has always been interested in solving women’s health challenges. For the past two decades, she’s been doing it on a global scale.
As co-director of the Rice360° Institute for Global Health Technologies, Richards-Kortum focuses her efforts on preventable conditions such as cervical cancer and newborn/infant mortality that disproportionately affect women in low-income areas.
Her lab develops imaging technologies than can rapidly diagnose health conditions in low-resource settings, such as a mobile imaging method that can diagnose and treat cervical precancer in a single visit. Cervical cancer is the fourth most common cancer in women globally with an estimated 604,000 new cases and 342,000 deaths in 20201.
Richards-Kortum also co-leads a global effort to eliminate preventable causes of newborn deaths in sub-Saharan countries. While most women in Africa deliver their babies in health facilities, nearly one million newborns die annually in sub-Saharan Africa2. These hospitals lack the life‐saving technologies, equipment, and trained staff to manage preterm babies and newborns in distress, explained Richards-Kortum.

To meet these needs, she and bioengineering professor Maria Oden, Ph.D. at Rice University co-founded the Newborn Essential Solutions and Technologies (NEST360°) partnership. This international team of leading clinical, biomedical, and public health experts from 22 institutions collaborates with local ministries of health, finance, and education to create strong neonatal intensive care units.
Richards-Kortum says interdisciplinary collaborative approaches are needed to solve big health challenges. “Introducing health care technologies in low-resource settings requires thinking about how we can strengthen the health care system. This is the kind of problem I find fascinating and rewarding to work on,” she said.
Her work in low-income countries has been recognized by several organizations. The American Institute for Medical and Biomedical Engineering selected her for its Pierre Galletti Award (2016), and Fortune Magazine named her as one the World's 50 Greatest Leaders (2017).
An accidental engagement
Richards-Kortum says she became involved in global health accidentally. “We were developing a new department of biomedical engineering at the University of Texas at Austin in 2000. I agreed to teach a biomedical engineering class for non-majors and then added a global health component to make the material more interesting to students who just wanted to fulfill their general science requirement.”
As she learned more about health inequities and saw the lack of biomedical engineers engaged in this area, she decided to change the focus of what her lab was working on—from technologies solving health problems in high-resource settings──to technologies solving health challenges in low-resource settings.
A visit to a pediatric AIDS clinic in Malawi in 2005 also informed her thinking about what the needs were.
“I saw nurses in newborn wards working so hard to care for babies without the necessary tools and technologies. At the same time, those hospitals had piles of equipment that broke because they could not withstand the harsh environmental conditions and couldn’t be repaired due to a lack of spare parts,” she said.
She returned to Rice University with a renewed commitment to thinking about what more could be done to support education and strengthen research in biomedical engineering in low-resource settings.
Richards-Kortum and Oden established the Rice360° Institute for Global Health Technologies in 2007 to offer educational opportunities to university students to design and implement new technologies to solve global health challenges. The institute also supports women-led research and ensures that engineers and experts from low-resource settings are included in the design and development process of new technologies.
Later in 2019, the NEST360° program was created by the co-founders working with a large international team. The goal is to design affordable, durable medical devices to sustain small and sick newborns in African hospitals. Among these devices has been an award-winning continuous positive airway pressure device for premature babies who struggle to breathe.
Point-of-care technologies
Her latest collaborative project is building a new NIBIB-funded center to develop point-of-care technologies that can diagnose oral and cervical cancers early when they are still treatable. The collaboration combines Rice’s technical expertise with the clinical/global health expertise of Baylor College of Medicine, the University of Texas Health Science Center, and the University of Texas MD Anderson Cancer Care in Houston. The team also includes technical and clinical partners in Brazil and Mozambique who help identify high priority needs and develop and implement effective solutions.
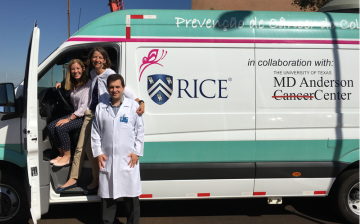
Photo courtesy of Rice University
Another goal of the new Center for Innovation and Translation of Point of Care Technologies for Equitable Cancer Care (CITEC) is to make cancer care affordable and accessible. Existing tests for early cancer detection are too complex and/or expensive to implement in primary care settings, particularly in medically underserved areas, explained Richards-Kortum.
CITEC is one of six centers included in the NIBIB-funded Point-of-Care Technologies Research Network that supports the development and acceleration of point-of-care technologies to meet unmet medical needs in the U.S. and globally.
Richards-Kortum, who was an inaugural member of NIBIB’s Advisory Council, said, “One of the things I love about NIBIB is that its supports technology development that’s making an important difference for women’s health and for health equity.”
Strengthening training
The NEST360º team has also partnered with local university engineering departments in Tanzania, Malawi, Kenya, and Ethiopia to create design studios (Maker Spaces) for project-based learning.

Credit: Brandon Martin, Rice University
“Their engineering curricula was strong, but it lacked project-based instruction. Now students and faculty are building technologies to address their local health needs,” said Richards-Kortum.
Examples of the technologies the students have developed include 80,000 face-shields during the COVID-19 pandemic and a model of the female reproductive tract that’s used in many countries, including the U.S., for hands-on training of health care workers in cervical cancer screening, early detection, and treatment at the point-of-care.
The NEST360° team has also collaborated with their partners to develop a pre-service and in-service training package to educate clinicians and biomedical technicians to use, maintain, and repair technologies to care for small and sick newborns.
“The training has had a positive impact; the equipment we delivered to these hospitals is functioning 90% of the time. This helps to eliminate those equipment graveyards that our team saw when we first visited Malawi,” said Richards-Kortum.
The future of women’s health
Despite progress being made in women’s health issues globally, many challenges remain.
“There is an important equity aspect to these issues. We have developed many tools already, but they’re often inaccessible to the people who would benefit from them. We need to make better technologies that are both affordable and accessible,” said Richards-Kortum.
She is encouraged by seeing more scientists, engineers, and health professionals making women’s health a priority.
“I see a lot of young women who are very dedicated to ensuring equitable access to health care, especially for women in under-served settings. That gives me hope for the future.”
Study References:
- World Health Organization. (2023) Cervical Cancer Fact-Sheet. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
- World Health Organization. (2019) Every Newborn Progress Report. https://www.who.int/publications/m/item/every-newborn-progress-report-2019
