- What is rehabilitation engineering?
- How can future rehabilitation engineering research improve the quality of life for individuals?
- What are NIBIB-funded researchers developing in the area of rehabilitation engineering?
What is rehabilitation engineering?

Rehabilitation engineering is the use of engineering principles to 1) develop technological solutions and devices to assist individuals with disabilities and 2) aid the recovery of physical and cognitive functions lost because of disease or injury.
Rehabilitation engineers design and build devices and systems to meet a wide range of needs that can assist individuals with mobility, communication, hearing, vision and cognition. These tools help people with day-to-day activities related to employment, independent living and education.
Rehabilitation engineering may involve relatively simple observations of how individuals perform tasks, and making accommodations to eliminate further injuries and discomfort. On the other end of the spectrum, rehabilitation engineering includes sophisticated brain computer interfaces that allow a severely disabled individual to operate computers and other devices simply by thinking about the task they want to perform.
Rehabilitation engineers also improve upon standard rehabilitation methods to regain functions lost due to congenital disorders, disease (such as stroke or joint replacement) or injury (such as limb loss) to restore mobility.
For more information on rehabilitation engineering at NIH, see https://www.nichd.nih.gov/publications/pubs/Documents/NIH_ResearchPlan_Rehabilitation.pdf
How can future rehabilitation engineering research improve the quality of life for individuals?
Ongoing research in rehabilitation engineering involves the design and development of innovative technologies and techniques that can help people regain physical or cognitive functions. For example:

- Rehabilitation robotics, to use robots as therapy aids instead of solely as assistive devices. Smart rehabilitation robotics aid mobility training in individuals suffering from impaired movement, such as following a stroke.
- Virtual rehabilitation, which uses virtual reality simulation exercises for physical and cognitive rehabilitation. These tools are entertaining, motivate patients to exercise, and provide objective measures such as range of motion. The exercises can be performed at home by a patient and monitored by a therapist over the Internet (known as tele-rehabilitation), which offers convenience as well as reduced costs.
- Physical prosthetics, such as smarter artificial legs with powered ankles, exoskeletons, dextrous upper limbs and hands. This is an area where researchers continue to make advances in design and function to better mimic natural limb movement and user intent.
- Advanced kinematics, to analyze human motion, muscle electrophysiology and brain activity to more accurately monitor human functions and prevent secondary injuries.
- Sensory prosthetics, such as retinal and cochlear implants to restore some lost function to provide navigation and communication, increasing independence and integration into the community.
- Brain computer interfaces, to enable severely impaired individuals to communicate and access information. These technologies use the brain’s electrical impulses to allow individuals to move a computer cursor or a robotic arm that can reach and grab items, or send text messages.
- Modulation of organ function, as interventions for urinary and fecal incontinence and sexual disorders. Recent developments in neuromodulation of the peripheral nervous system offer the promise to treat organ function in the case of a spinal cord injury.
- Secondary disorder treatment, such as pain management.
What are NIBIB-funded researchers developing in the area of rehabilitation engineering?
Promising research currently supported by NIBIB includes a wide range of approaches and technological development. Several examples are described below.
Navigation aids: Blind individuals require assistance to navigate through unfamiliar locations. Researchers are developing a cane that is enhanced with computer vision and vibration feedback. The cane uses advanced image processing to map the structure of a room, identify important features (door, stairs, obstacles), and create a navigation plan to guide the user towards his destination. It provides feedback in the form of either speech or vibrations through the handle.
Another group of researchers has developed a device that provides very low resolution images to the user. The system consists of a retinal implant, a pair of glasses containing a small camera, and a cell phone-sized device to convert the camera’s images into digital signals. The system provides electrical stimuli to the retina, which sends nerve impulses through the optic nerve to the brain. The resulting images observed by the user provide just enough information about the environment to navigate through a room and read large writing, such as street signs. The researchers are performing pre-clinical studies to attain FDA approval to run a Phase I safety trial.

Restoring muscle control: People with spinal cord injuries have limited or no ability to control muscle groups below the site of the injury. This often requires assistive mobility devices (crutches, wheelchairs, or powered wheelchairs) and part- or full-time caregiver support. One research team is investigating a technological approach to bypass the injury. They have built a fully-implantable system that uses a sensor to measure voluntary muscle contractions above the injury; the sensor in turn sends electrical signals to trigger muscle activity below the injury. The technology has enabled restoration of standing, stepping, cycling, and hand grasp. Another research team is using electrical stimulus in conjunction with physical therapy to more effectively train the central nervous system to enhance the function of the few remaining neurons at the site of the injury. The team uses a completely non-invasive system to train the nervous system below the injury how to walk. This approach has improved walking speed long after the therapy has ended. Another approach uses implantable spinal cord stimulators, originally designed to reduce pain, to alter the neural activity in the spine to restore control of standing and stepping in patients. All of these teams are planning to attain FDA approval for Phase I safety trials.
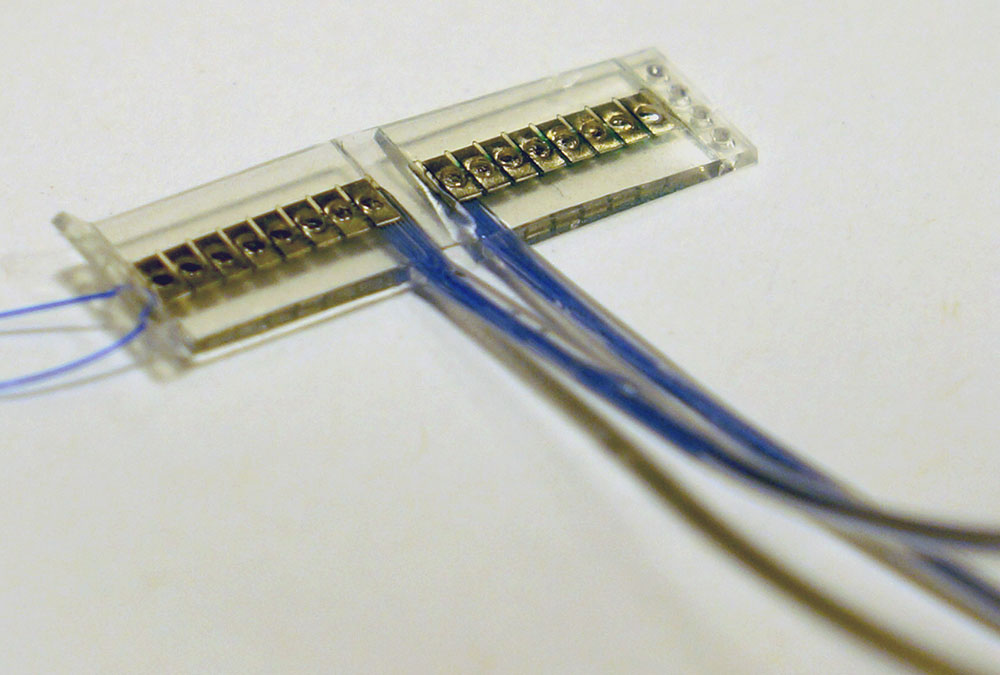
Prosthesis control: Standard-of-care prostheses for amputees, while increasing in sophistication, lack the ability to reliably detect a user’s fine motor commands. Several teams are developing technologies to more accurately record and transmit the user’s intent to use their hands to grasp, grip or pinch by recording the electrical signals sent by the user. By implanting electrodes in the residual arm muscles, peripheral nerves, spinal cord, and brain, it is possible to detect these electrical signals, convert them into digital commands, and drive the motors in a hand prosthesis to significantly improve function. Researchers are fine-tuning the system for each limb as well as the different needs of each amputee. By exploring all of these approaches simultaneously, it should be possible to advance the state of the art faster. Several studies have FDA approval for clinical trials, and the others are still undergoing preclinical research prior to advancing to trial.
Closed-loop braces for limbs, spine: Traditional orthoses, or braces, were purely mechanical, passive devices to provide structural, postural, and functional characteristics of the musculoskeletal system. By incorporating electronic sensors, controllers, and motors, it is possible to greatly increase functional performance for users. One approach is to build an ankle-foot brace with a hydraulically adjustable stiffness to mimic the muscles and tendons in a healthy individual. This team is developing a child-size version of the device, which adjusts to maintain a proper fit as the child grows. Another approach is to develop a hydraulic system to use forces from a user’s un-impaired or less-impaired limb to support motion by the impaired limb. And yet a third approach is to build an electromechanical control system capable of supporting a complete range of motion for individuals with thoracic/lumbar vertebrae that are compressed or crushed.
Updated November 2016
