- What are drug delivery systems?
- How are drug delivery systems used in current medical practice?
- What technologies are NIBIB-funded researchers developing for drug delivery?
What are drug delivery systems?
Drug delivery systems describe technologies that carry drugs into or throughout the body. These technologies include the method of delivery, such as a pill that you swallow or a vaccine that is injected. Drug delivery systems can also describe the way that drugs are ‘packaged’—like a micelle or a nanoparticle—that protects the drug from degradation and allows it to travel wherever it needs to go in the body. The field of drug delivery has advanced dramatically in the past few decades, and even greater innovations are anticipated in the coming years. Biomedical engineers have contributed substantially to our understanding of the physiological barriers to efficient drug delivery and have also contributed to the development of several new modes of drug delivery that have entered clinical practice.
Yet, with all of this progress, many disease treatments still have unacceptable side effects. Side effects occur because drugs interact with healthy organs or tissues, and this can limit our ability to treat many diseases such as cancer, neurodegenerative diseases, and infectious diseases. Continuing advances in this space will help to facilitate the targeted delivery of drugs while also mitigating their side effects.
How are drug delivery systems used in current medical practice?
Clinicians historically have attempted to administer interventions to areas of the body directly affected by disease. Instead of delivering drugs systemically, which affects the whole body, some drugs can be administered locally, which can decrease side effects and drug toxicity while maximizing a treatment’s impact. A topical (used on the skin) antibacterial ointment for the treatment of a localized infection or a cortisone injection to relieve pain in a joint can avoid some of the systemic side effects of these medications. There are other ways to achieve targeted drug delivery, but some medications can only be given systemically.
Another example of a drug delivery system includes the components of a vaccine that helps it to travel inside the body. Vaccines work by providing our immune system with instructions to recognize and attack a pathogen. These ‘instructions’—such as mRNA, in the case of some COVID-19 vaccines—must be packaged so that it is not degraded by the body and can reach its target. The packaging used for COVID-19 mRNA vaccines are lipid nanoparticles, which protects the fragile mRNA cargo and facilitates its delivery into cells.
What technologies are NIBIB-funded researchers developing for drug delivery?
Current research on drug delivery systems can be described in two broad categories: routes of delivery and delivery vehicles.
Routes of Delivery
Medications can be taken in a variety of ways—by swallowing, by inhalation, by absorption through the skin, or by injection. Each method has advantages and disadvantages, and not all methods can be used for every medication. Improving current delivery methods or designing new ones can enhance the use of existing medications.
Microneedle patch for painless vaccinations: Microneedle arrays are one example of a new method to deliver medications through the skin. In these arrays, dozens of microscopic needles, each far thinner than a strand of human hair, can be fabricated to contain a medicine. The needles are so small that, although they penetrate the skin, they don’t reach the nerves and can deliver medications painlessly.
NIBIB-funded scientists are developing such a patch with an array of dissolvable microneedles for vaccine delivery. These patches are easy to use and do not require refrigeration or special disposal methods, so they could be used by patients at home. This technology could be especially helpful in low-resource communities that may not have many health care providers or adequate storage facilities for traditional, refrigerated medicines.

Robotic pill for oral drug delivery of complex drugs: Self-injections are used to manage some diseases, such as diabetes and Crohn’s disease. Medications for these conditions may require an injection because the drugs used are often complex and easily degradable, and therefore can’t be taken orally. However, self-injection can represent burdens for patients, including the frequency of the injections and the potential for needle stick injuries.
NIBIB-funded scientists are developing an alternative method for self-injection: a robotic pill that can be loaded with complex, liquid drugs. Once swallowed, this pill makes its way to the stomach, where the drug is injected into the stomach tissue. The pill is then excreted through the gastrointestinal tract. While these robotic pills have only been evaluated in animal models so far, they could potentially offer an alternative to self-injection across a range of conditions.
Delivery Vehicles
Drug delivery vehicles represent different ways that medications can be packaged so that the drug can safely travel within the body. Some common examples of drug delivery vehicles include micelles, liposomes, or nanoparticles. Different drug delivery vehicles can improve the targeting of the drug by helping the medication travel exactly where it needs to go. Additionally, research in this space allows for the development of new ways to package hard-to-use drugs, for reasons like size or fragility. These improvements in biotechnology are leading to improved medications that can target diseases more effectively and precisely.
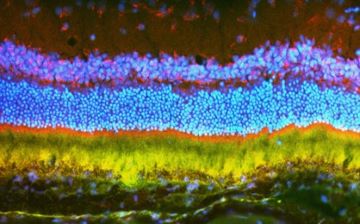
Nanoparticle carriers for the treatment of eye disorders: Gene transfer therapies—where genetic material that codes for therapeutic proteins is introduced into cells—represent a promising way to treat a variety of eye disorders, including macular degeneration. Current delivery methods have limitations, such as the size of the genetic material that they can hold, and their tendency to initiate an immune response.
NIBIB-funded scientists are developing a nanoparticle to carry genetic material that overcomes these limitations. These nanoparticles are not readily detected by the immune system and can hold larger genes than current methods. In a mouse model of macular degeneration, the researchers found that injection with their gene-loaded nanoparticles resulted in a 60% reduction in abnormal blood vessels (a characteristic of the disease that causes vision impairments) compared with controls. While still in the early stages, this research could lead to better treatments for eye disorders.
Mimicking immune cells to combat inflammation: While inflammation is an essential part of our immune response to harmful substances, excessive inflammation in the vascular system can ultimately cause tissue injury, notably in the lungs. Acute respiratory distress syndrome (ARDS) is a life-threatening condition characterized by sudden and severe damage in the lungs which can cause low blood oxygen levels. Treatments typically include mechanical ventilation, but there are no recommended pharmacological interventions. Mortality rates for ARDS are high, ranging from 35-46%.
Part of the vascular inflammation process includes the migration and adhesion of neutrophils, a type of immune cell, into the lungs, where they bind to endothelial cells. Taking advantage of this behavior, NIBIB-funded researchers are designing nanovesicles that mimic neutrophils, which could be loaded with anti-inflammatory drugs that then deposit their therapeutic cargo in the lungs. This new drug delivery system, inspired by biology, is still early in development.
Updated July 2022
